The quick update: My scans from August looked “fine” (the cancer is not growing, no progression) and my tumors marker bloodwork from this month showed improvement. Lower numbers are better and mine dropped so that is also encouraging!
So, we celebrate!
I’ve been fortunate to have the opportunity to travel (work and pleasure) and generally feeling good. Generally.
I had to go to Pasadena for work and stayed for the weekend. Maddy flew out to join me and we spent the Labor Day weekend with my BFF. We played tourist on Saturday in the 100+ degree heat.

It’s amazing to reflect back on time – Laura and I met when I went to grad school in Davis, CA. She needed a roommate and I needed a place to stay. That was 1993 – before social media, before cell phones. We had a phone call – I think – and that was it. We were roommates. Little did I know I was gaining a fourth sister!
It’s because of science that I’m able to spend time with her and her daughter. Science that has let me live a pretty “normal” life since this diagnosis of stage IV (metastatic) breast cancer. If this were 2010 or even 2015, the conversation would be very different. I would not be creating these new memories. I’d be recovering from chemo that probably would not work very long.
I sound like a broken record – live your life. Really. Do those things that have meaning and will matter to you a year or 5 years or 10 years from now. It’s way too easy to get caught up in the day to day and slide through life.
~~~~~~
Longer science-y version
I withdrew from the clinical trial. I decided I was not comfortable with not knowing if I was getting medication or the placebo. To be clear, I was getting the standard of care – meaning that I was getting the medication that is normally prescribed.
On Wednesday of last week (5 days ago) I re-started Ibrance, the CDK 4/6 inhibitor that I was on before. This is paired with a drug that blocks estrogen. That drug for me now is a shot called Fluvestrant (or Flaslodex). The shots don’t bother me so much when I get them. I haven’t had much in the way of side effects – or so I thought. I’m thinking this shot is messing with my back.
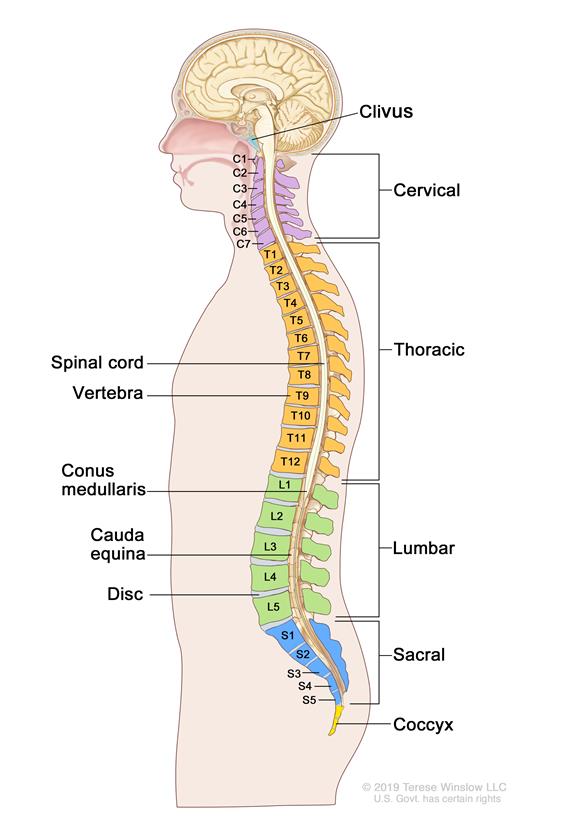
The past few months I’ve had sporadic pain in my lower back. So much so that it’s hard to move around, even walk. It’s hard to pinpoint what is happening, but I’m now thinking there might be a correlation and this is a side effect. (I actually had an episode this past weekend that lasted 24 hours during which I could barely stand up and walk.)
Fluvestrant is a “Selective Estrogen Receptor Degrader” (a SERD). This means that it messes with the estrogen receptor on cells. You can think of the receptor as the thing the estrogen attaches to. It’s kind of like a docking station. This medicine messes up the docking station so when the estrogen tries to attach to a cell it can’t. My cancer feeds off estrogen – if it can’t connect to the estrogen, it can’t proliferate and grow.
Previously I was on a different drug that prevented the creation of estrogen. The thought is that the cancer figured out what was going on and found a way to work around that to grow. So, I had to switch treatments.
Hopefully this SERD will work and for a long time!
I also continue to get an infusion of a bone strengthener every three months (Zometa). I had my infusion on Wednesday also. My veins tend to roll and are not easy to get an IV into. I thought a new nurse hit the jackpot until the saline started going into my arm. Nothing major, but it was uncomfortable and they had to try a different location for the IV. Certainly not the end of the world but one of those things you deal with living in Cancerland.


~~~~
Current meds: Ibrance (125 mg), Fluvestrant, Zometa, Lupron