June 4, 2025
Happy summer my friends. In Colorado we are starting off with a cool, wet one which is great for the a/c bill but less ideal for exploring outside.
Lot’s going on here including medically.
I had some work travel last month and towards the end I started not feeling well, including being light headed. I mentioned this to my oncology nurse 2 days ago during my treatment appointments and she scheduled a brain MRI and echocardiogram. Yes, light headedness triggers the immediate thought of brain metastasis.
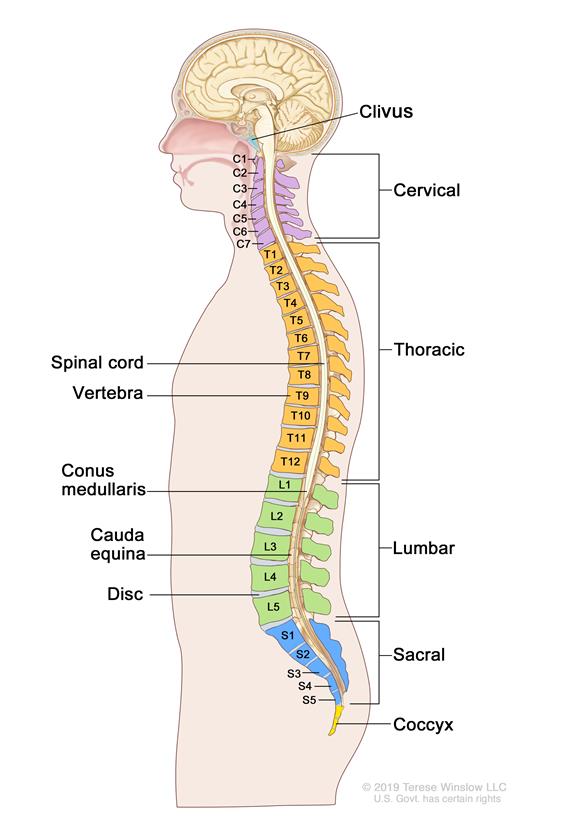
Recall from my last post that we’ve found the MRI to be the best imaging for me. The brain MRI captures the head and top part of the spine (cervical). Mixed results: no brain metastasis 🙌 but it did pick up a new lesion on my C1 vertebrae 👎.
The nerves that come out of the C1 impact the sides of your face and head as shown in this nifty diagram (one of my fav diagrams BTW).
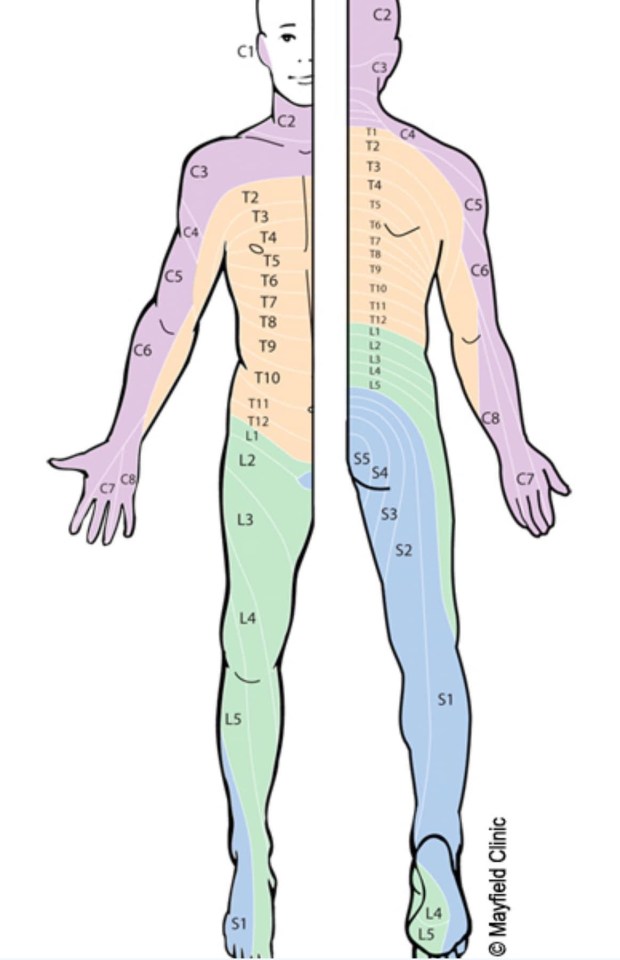
The most likely explanation for my light headedness is that the lesion (tumor) is pressing on the nerves. So, my oncologist has ordered another PET/CT to check again. It seems a little insane to keep getting imaging that doesn’t work so well – I guess he wants to confirm or look for other lesions.
My tumor markers did drop the end of last month which is in contradiction to the new tumor.
See how complicated and tricky cancer is?
For now, I’ll get the PET/CT and an echocardiogram and keep doing all the things (eating healthy, moving, relaxing) and we shall see where this takes me.
After my work trip I spent 2 days in Chicago at the American Society for Clinical Oncology (ASCO) where I learned about new treatment lines coming out and connecting with other patient advocates.
The cancer research going on now will result in the drugs being used in the coming years. This is why it is so important to preserve funding for the National Institutes of Health. The presidents budget slashes funding by almost 50%. That means many fewer clinical trials and many fewer drugs in 5 years. No one expects to get cancer. If you get cancer in 5 years you will be wishing the NIH had done more research to help you. Please call your elected federal reps and push for restoring funding to NIH.
On a lighter note – Maddy graduated from high school, Evelyn started a research internship at University Colorado Anschutz Medical Campus and we all head to Las Vegas at the end of the month to support Maddy in her last National Dance Competition.
Onward!