October 11, 2025
September was a busy month for me in managing cancer.
Back in June I had a brain MRI, which includes the very top of your spine (cervical). At that time, it looked like there might be an active tumor in part of my C1 vertebrae. I also had a full body PET scan that showed “stable” cancer at the time (mainly my spine has been problematic).
The stable PET scan means that my treatment (Enhertu) is largely working. However, the tumor on my C1 made me nervous. Your C1 is directly at the back of your head at the height of your nose. If anything goes wrong there it can be complicated and in the words of my oncologist “catastrophic” 😳
After discussing with my oncologist in August, we decided to radiate it. It’s not uncommon with metastatic breast cancer (MBC) to consider radiating smaller tumors if everything else is stable or no evidence of disease (NED).
So, I decided to pack this in to September which was already busy.
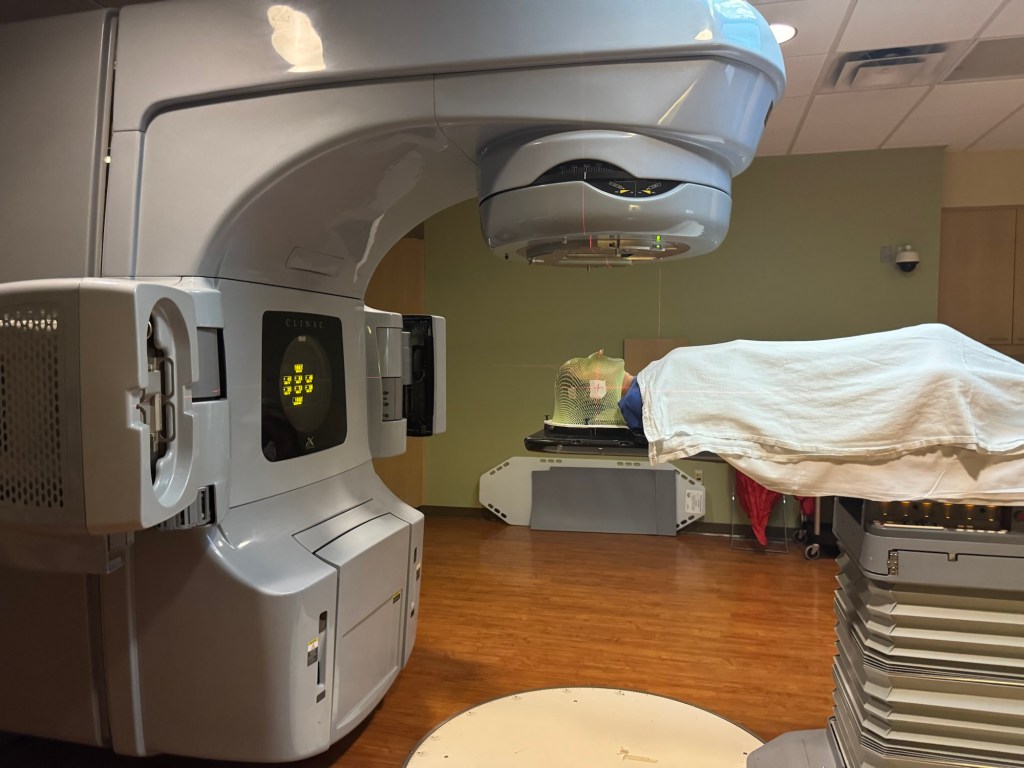
After another MRI of my cervical spine I met with a radiation oncologist. He wanted to do Stereotactic external Beam Radiation Therapy (SBRT) – a concentrated radiation that would have been 2 sessions.
My insurance company disagreed with my radiation oncologist and wouldn’t cover it.
I could appeal it but that can take weeks and I didn’t want to give the tumor more time to get comfy and grow. So instead, I had to go for 10 sessions over two weeks.
You have to lay perfectly still for radiation so that the beam hits the intended target. At my planning session appointment they created a mask. A mesh of warm plastic was placed over my face and head and molded to my exact shape. The photo of the mask shows me with a big smile – not that I’m super happy to be doing this, I just naturally smile for photos.

Then I got out of town. Drove Maddy to Cal Poly and then back home. The next day I jumped on a plane to Providence for work. Glen flew out at the end of the week and we spent the weekend (our first as official “empty nesters”) with my cousin playing tourist.

We got home late on a Sunday and Monday morning at 9am I had my first radiation treatment.
The photo shows me right after they finished a treatment. The mask mostly feels like a heavy blanket with a lot of holes draped over your head.
I had 10 treatments (M-F) over two weeks. Within those 2 weeks I also had my Enhertu infusion and got my flu and COVID boosters.
As soon as I finished radiation I headed back to the east coast, Washington DC this time to advocate on the Hill for funding for cancer research.
It’s been a lot, however, I refuse to let cancer dictate my life. Most of those days I was in bed before 9pm. I’m grateful that my side effects are minimal and I can still do “all the things”.
The side effects of radiation to your head are not pleasant. This week I developed a wicked sore throat to the point that I couldn’t swallow. Food doesn’t taste like anything. My fatigue has been ridiculous.
October is a little more quiet but more travel for work and fun.
I hope you all are living your best life and doing the things that make you happy and matter to you, whatever that might be.
Onward!