October 13, 2025
Today is Metastatic Breast Cancer Awareness Day. We get this one day in breast cancer awareness month to shine a light on MBC.
1 in 3 of women cured of breast cancer
will be diagnosed as stage IV (MBC), which is terminal.
If we cure Stage IV, we cure all breast cancer.
In support of raising awareness for MBC, I went to Washington D.C. last week and participated in the METAvivor Stage IV Stampede and Summit.
The Summit included a day of education about MBC as well as how to advocate for various bills and funding.
Tuesday we marched (with police escort) from our hotel to the Capitol. We had a remembrance on the grass. I am holding the sign on the end, near the last “R”. We spoke the names of those who have died from MBC (and I included my aunt Jeanne Moretti as well as several other friends who have passed).

We met with staffers of our elected representatives. Staffers were taking meetings even though the House was not in session and the federal government was/is closed.


There were four “asks” that we made. I had fantastic interactions and felt like I was heard. I’ll share here what those asks were – if you feel compelled to share with friends/family or to reach out to your own elected representatives that would mean a lot.
- Did you know that if you have MBC and need to stop working there is 5-month waiting period for Social Security Disability Insurance (SSDI) benefits to start? In addition, after that there is a 24-month waiting period before you are eligible for Medicare! I am one of the fortunate people who is living longer with my MBC diagnosis and can still work. Women with different subtypes have a prognosis of 2-3 years. During this time they can’t work and can’t get SSDI or Medicare. House bill 2048 “Metastatic Breast Cancer Access to Care Act” would eliminate the waiting period.
- Did you know that where you live impacts how private insurance pays for MBC drugs? Private insurance treats medication received at a cancer center different from medication taken at home. Recall that I was on a pill (Ibrance) for the first 4 years. I live in a state where private insurance is required to pay for this (chemo) regardless of how it is given: intravenous or a pill. House bill 4101 (Cancer Drug Parity Act) would require private insurance to cover oral cancer drugs the same as IV drugs, regardless of what state you live in.
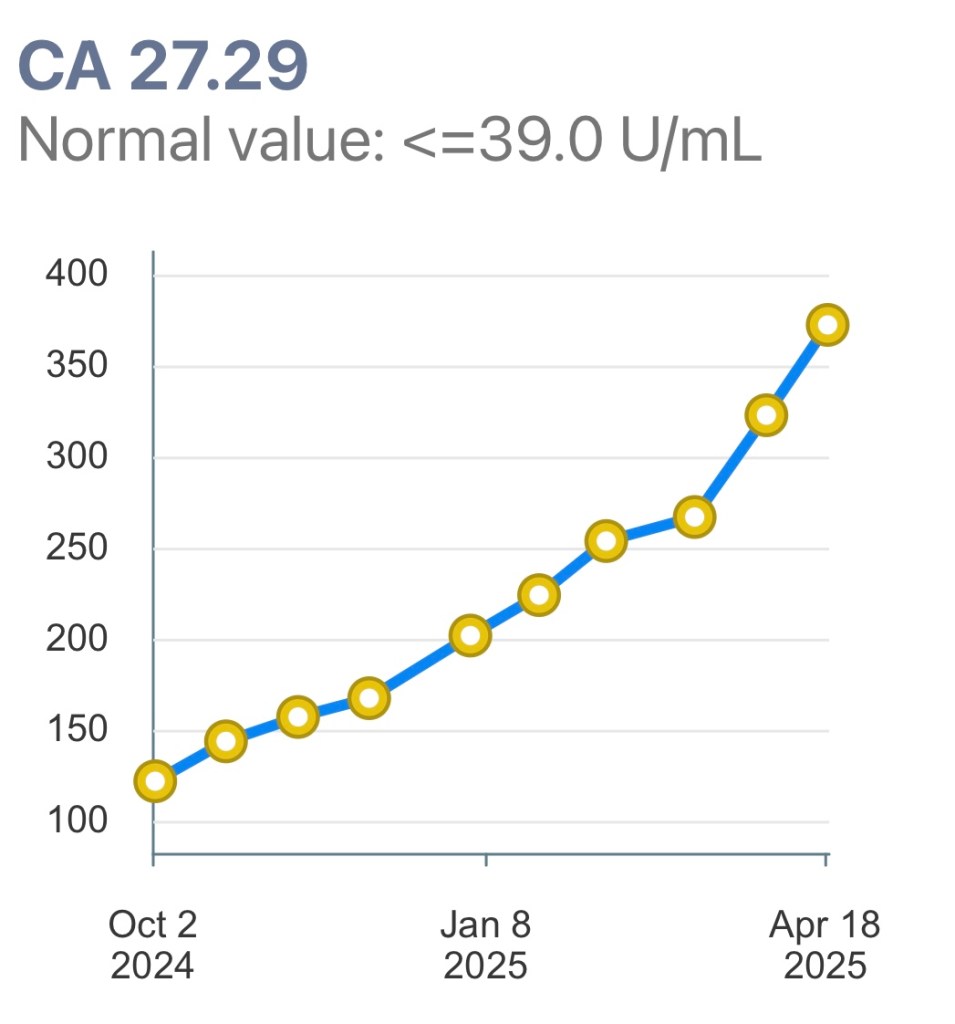
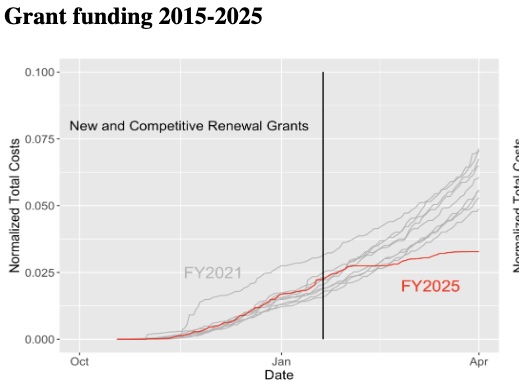
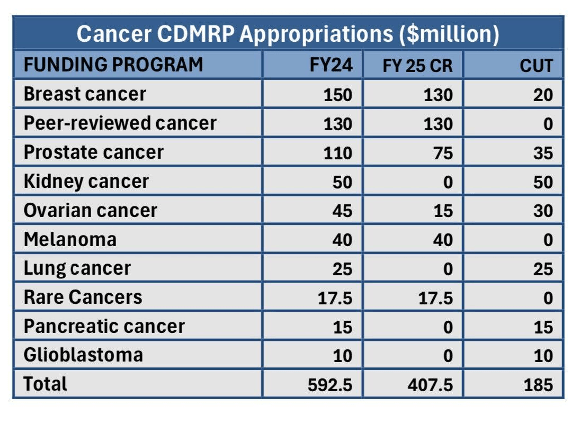
- The U.S. is the largest funder in the world of cancer research. The administration’s budget zeroed out some breast cancer research programs and greatly reduced funding for the National Institutes of Health (NIH). Fortunately, Congress likes science – we asked them to provide the NIH with the same funding as last year and restore the breast cancer program in the Dept. of Defense.
- Did you know there is a national database of incidence of cancer? It was created in the ‘70s during the Nixon administration. Unfortunately, it has not been updated since then. The Surveillance, Epidemiology and End Results (SEER) database provides information on cancer statistics which is used to inform where research dollars should go. It needs to be updated badly and I asked our reps to support funding for it. SEER help us understand where there is a high burden of cancer. It turns out that not every state is contributing to it. In addition, it does not include any recurrence of cancer. When I was first diagnosed, my information was put into SEER (LCIS and stage 0 DCIS breast cancer). However, there is no mechanism to update my information! According to SEER I was treated in 2009 and all is good with me. As you can see, the number of people with MBC or with any recurrent cancer are not counted which means we have no idea who is living with metastatic disease (unless you were diagnosed with MBC right away, which is only 6% of all MBC diagnoses).
That was a lot! If you are still reading, thank you. If you’d like more information about anything including language to send to your elected representatives, shoot me an email (charlevo@gmail.com).
I have one other cancer event this week and then I will take a break from cancer the rest of this month. I hope you are keeping balance in your life as well.
Onward!
1. Donate to research for MBC via METAvivor.